


In recent years, the healthcare industry has experienced a transformative shift, moving from traditional tools and machines to advanced artificial intelligence (AI) solutions. This evolution is reshaping how care is delivered and managed worldwide.
The integration of AI in healthcare matters today more than ever, due to its potential to enhance medical outcomes, reduce costs, and streamline operations, addressing pressing social and economic challenges.
Tools like IBM Watson Health analyze vast amounts of medical data, identifying patterns and aiding doctors in developing personalized treatment plans. This capability improves early diagnosis and treatment accuracy, significantly enhancing patient outcomes.
Meanwhile, Olive AI's automation of back-office tasks frees up resources, reduces human error, and speeds up processes, contributing to more efficient healthcare delivery systems. This technological growth offers practical solutions to longstanding administrative bottlenecks.
The evolution of healthcare technologies underscores the critical role AI plays in advancing medical care, providing actionable benefits like improved diagnosis, cost-efficiency, and streamlined operations, which pave the way for optimized health services.
Understanding the evolution of healthcare technologies offers insights into today's advancements. The journey from rudimentary tools to high-tech solutions reveals endless innovation aimed at improving health services.
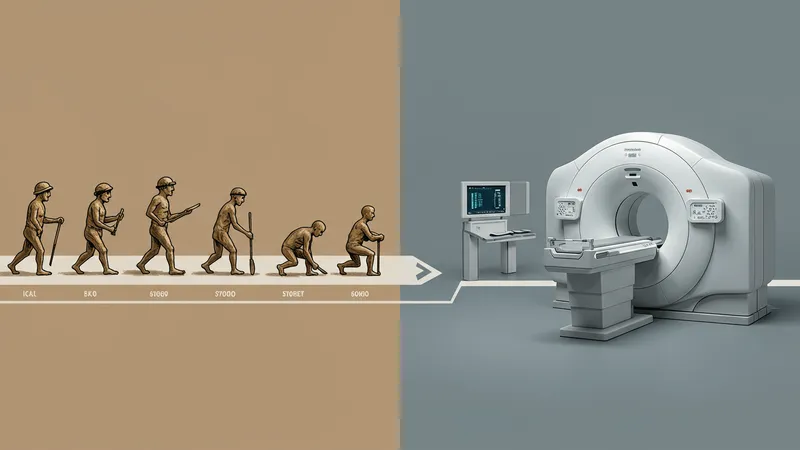
Initially, healthcare relied on simple instruments, evolving into complex machines like MRI and CT scans, which revolutionized diagnostics by providing clearer, more accurate images of the human body.
The introduction of digital health records marked another turning point, enhancing data management and patient care coordination. This digitization laid the groundwork for current AI integration.
As technology progressed, AI emerged as a game-changer, facilitating advanced data analytics and insights, heralding a new era of precision medicine that continues to evolve today.
AI systems excel in diagnostics by evaluating vast data sets to reveal patterns unseen by the human eye. These capabilities enhance accuracy and speed in diagnosing conditions, significantly improving patient outcomes.

AI-powered imaging tools, such as those developed by Aidoc, help radiologists detect anomalies efficiently, facilitating early disease intervention. Improved diagnostic processes reduce misdiagnosis risks and expedite treatment.
Moreover, AI solutions provide predictive analytics that identify potential health risks before they manifest, offering proactive healthcare management that can save lives.
For healthcare professionals seeking to improve diagnostic accuracy, embracing AI technologies offers promising potential to transform their clinical practices.
The ability to customize treatment plans is a standout feature of AI technologies. By analyzing individual patient data, AI engines help tailor therapies to match personal health profiles.
Platforms like Tempus use AI to sift through genetic information and previous medical history to recommend personalized cancer treatments, improving efficacy and patient response rates.
This personalized approach reduces the trial-and-error aspect of traditional treatments, allowing doctors to devise precise plans, potentially enhancing recovery and quality of life.
As AI continues to evolve, its capacity to revolutionize treatment protocols is immense, offering hope for more targeted and effective intervention strategies across various medical fields.
AI adoption in healthcare not only improves clinical outcomes but also offers significant cost advantages. By automating repetitive tasks, AI reduces labor costs and minimizes errors.

For example, AI-driven solutions like those from LeanTaaS optimize hospital resources, improving scheduling and resource allocation, which in turn mitigates wastage and reduces operational costs.
Hospitals leveraging AI for supply chain management witness lower administrative costs, freeing up capital for patient care improvements and innovative technologies.
Investing in AI technology is being increasingly regarded as a cost-saving measure with potential long-term financial benefits for health institutions globally.
Robust data management is essential for modern healthcare facilities, ensuring efficient operations and informed decision-making. AI technologies excel at handling and analyzing vast data volumes.
Platforms like Google Health use AI to integrate and synthesize medical data, enhancing information accessibility and utility for clinicians and researchers alike.
Improved data management facilitates continuity of care, enabling seamless updates to patient records and historical tracking, which are critical for comprehensive healthcare delivery.
Efficient AI-powered data solutions are now indispensable tools, driving healthcare forward in an increasingly data-reliant world.
Patient engagement is crucial for successful treatment outcomes and long-term health management. AI tools empower patients with knowledge and participation in their care.

Chatbots and virtual assistants provide 24/7 support, answering questions and guiding patients through healthcare processes, making health resources more accessible.
AI-enhanced applications, such as those from HealthJoy, deliver personalized health insights, encouraging proactive patient involvement and adherence to treatment plans.
Implementing AI for patient engagement creates a more patient-centered approach, enhancing satisfaction and compliance, ultimately boosting healthcare results.
As AI technologies permeate healthcare, addressing ethical concerns becomes crucial for trusted implementation. Issues like data privacy, consent, and algorithm bias need vigilant management.

Healthcare providers must adhere to rigorous standards and policies ensuring patient information's ethical use, safeguarding privacy while benefiting from AI advancements.
Stakeholders collaborate to establish clear, fair guidelines that protect patient rights while allowing technological growth. Feedback loops and transparent algorithms are essential.
Balancing innovation with ethical responsibility remains a pivotal aspect of AI's integration into healthcare, requiring ongoing dialogue among experts, regulators, and patients.
Successfully deploying AI in healthcare involves strategic planning and execution. Establishing clear goals, stakeholder engagement, and selecting suitable technologies are foundational steps.

Healthcare organizations should pilot projects before full-scale implementation, ensuring that AI solutions align with clinical objectives and patient needs.
Continuous training and adaptation among staff are vital, fostering a culture that embraces AI capabilities and optimizes technology use.
Best practices in AI adoption ensure sustainable integration, maximizing the benefits of technological advances in healthcare settings.
The future of AI in healthcare looks promising, with potential expansions in areas like robotics, telemedicine, and genomics. Continued research will unlock further applications and efficiencies.
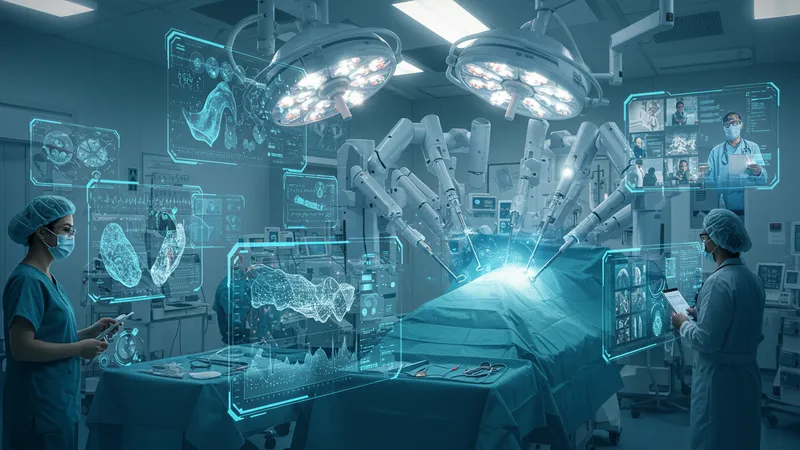
Emerging AI advancements can automate surgical tasks, enhancing precision and safety, while telemedicine platforms broaden access to care, transcending geographical barriers.
AI's role in genomics promises breakthroughs in understanding genetic diseases, offering hope for personalized treatment and prevention measures at the genetic level.
The trajectory of AI in healthcare continues to unfold, promising innovative solutions to meet evolving global health challenges, benefiting patients and providers alike.
As we conclude our exploration, the transformative potential of AI in revolutionizing healthcare becomes evident. By improving diagnostic accuracy, personalizing treatments, reducing costs, and enhancing patient engagement, AI is reshaping the industry. It's crucial for healthcare stakeholders to embrace these technologies responsibly, balancing innovation with ethical considerations. The journey of AI in healthcare is just beginning, and it promises a future where medical outcomes are significantly improved and accessible. To stay informed and adapt to these changes, healthcare professionals and organizations must continue exploring AI's capabilities, ensuring that advancements lead to enhanced patient care and operational efficiency.