

Imagine a bustling hospital where every urgent test and screening can happen bedside, without the delays of transporting samples or patients. That’s the promise of portable clinical diagnostic devices tailored for large healthcare environments. These advanced instruments are designed to deliver accurate, on-the-spot diagnostic results—right where the care happens—helping clinicians make faster, more informed decisions for a high volume of patients. In a country like Mexico, where regional hospitals serve dense urban populations and remote communities alike, portability and scalability of diagnostic tools play a critical role in modern healthcare delivery.
Portable clinical diagnostic devices encompass compact, mobile testing systems capable of analyzing blood, urine, and other specimens, as well as imaging tools that travel to the patient. For Mexico’s high-capacity facilities, these technologies are transforming routine lab work, triage, and even emergency care. They offer rapid results and integrate with digital medical records, streamlining workflows for clinicians—from major city hospitals to rural clinics aiming to reach more patients with fewer resources. Now, let’s explore key devices driving this transformation in Mexico’s busiest hospitals and clinics.
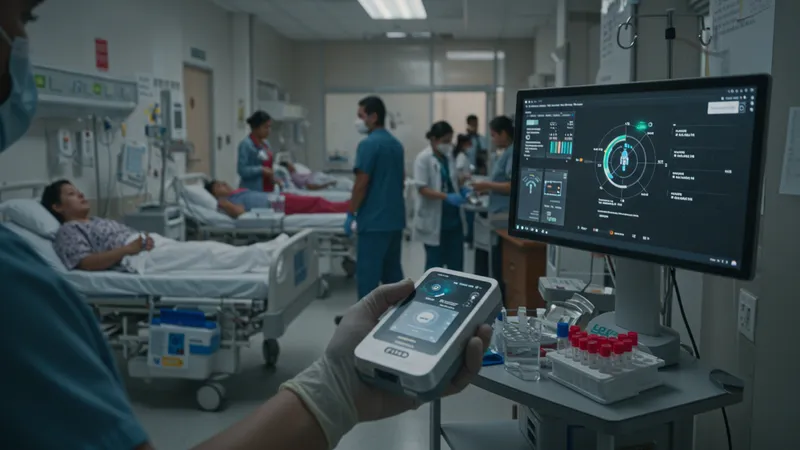
The increasing reliance on portable diagnostic tools in Mexican facilities stems from both urban and rural healthcare dynamics. In metropolitan hospitals, managing surges in patient volume means laboratories are often stretched thin. Here, devices like the Abbott i-STAT Alinity and Siemens Atellica Solution help alleviate central lab bottlenecks by bringing reliable testing to point-of-care locations within the hospital floor. Speedy test turnaround can be decisive during emergencies, trauma cases, or busy flu seasons.
Meanwhile, the Cepheid GeneXpert Xpress is making big strides in infectious disease management. During periods of heightened viral threats, such as the COVID-19 pandemic, Mexican hospitals have relied on the Xpress system’s portability and accuracy for onsite outbreak containment and rapid diagnostics, ensuring high throughput without overwhelming core labs. For clinicians, this translates into actionable data within minutes, critical for both patient care and epidemiologic control.
The EKF Biosen C-Line’s glucose and lactate readings offer a lifeline for diabetic and intensive care units filled to capacity. Mexico’s hospitals have some of Latin America’s highest diabetes caseloads; portable analyzers allow bedside monitoring and timely interventions, improving clinical outcomes and efficiency. Furthermore, the accessibility and lower price point make these vital tools for expanding capacity in public hospitals.
Portable ultrasound scanners like the Dragonfly Mini enable non-invasive imaging for trauma, obstetrics, and cardiology even in resource-limited environments. Applications range from crowded urban ERs to transport in rural mobile clinics, democratizing patient access to real-time visualization and specialist consultations. This rapid mobility reduces wait times, expedites diagnoses, and enables more equitable healthcare experiences, regardless of geography.
In summary, Mexico’s high-capacity healthcare facilities are integrating these five portable clinical diagnostic devices to manage soaring patient demands, speed critical decision-making, and bring quality care to every corner of the hospital. But how do these technologies compare in terms of scalability, maintenance, and integration with digital health systems? The deeper details reveal even more valuable insights ahead…
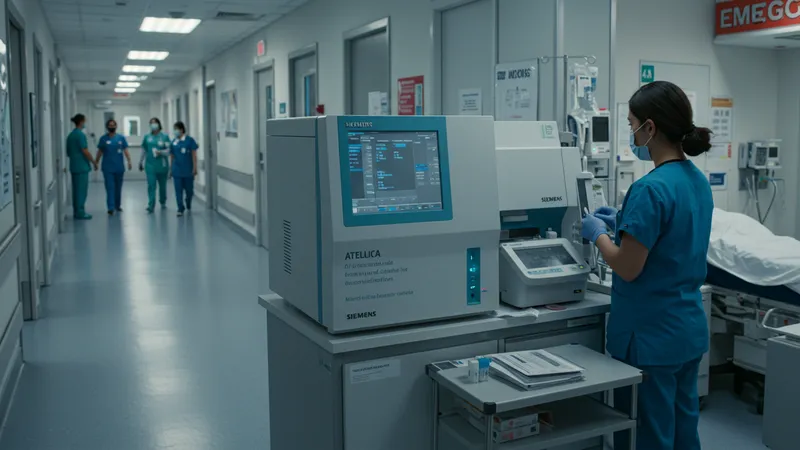
The varied workload across Mexico’s largest hospitals demands that portable diagnostic devices excel in both accuracy and adaptability. Devices like the Siemens Atellica Solution stand out, as they can be configured to handle both centralized high-throughput lab testing and decentralized near-patient analysis. This modularity allows institutions to adjust to surges, such as during epidemics or large-scale emergencies, while maintaining consistent quality controls essential for clinical governance in high-capacity environments.
One of the defining features of the Abbott i-STAT Alinity is its swift result delivery—critically important in emergency and intensive care units where patient turnover is high. The i-STAT’s ease of use and robust design allow nurses and paramedics to perform tests with minimal training, facilitating immediate interventions for trauma or cardiac incidents. This efficiency can increase the number of patients effectively treated per shift and supports rapid medical decision-making in Mexico’s urban hospital corridors.
For infection prevention and outbreak response, the portability and contained workflow of Cepheid GeneXpert Xpress systems have allowed Mexican facilities to establish isolation zones and rapid triage points. Especially in pandemic scenarios, its ability to provide SARS-CoV-2, tuberculosis, and influenza diagnostics within under an hour has reduced cross-contamination risks and protected both staff and vulnerable patient populations.
The EKF Biosen C-Line’s minimal maintenance needs and user-friendly interface are particularly valuable for resource-constrained hospital wings where laboratory techs rotate quickly, and the patient census is persistently high. Its reliable glucose monitoring particularly benefits Mexico’s diabetes care infrastructure, where fast, on-site measurements can prevent complications and unplanned admissions. Up next, we will explore pricing and total cost of ownership in the Mexican context.
The investment required for portable clinical diagnostic devices varies widely, with initial unit costs and longer-term maintenance playing crucial roles in budgeting for Mexico’s healthcare administrators. For instance, while the Siemens Atellica Solution carries a higher upfront price, its versatility and high-volume throughput can justify the expense for flagship hospitals aiming to centralize and decentralize laboratory functions fluidly. The modular build also helps control future upgrade costs as technology evolves.
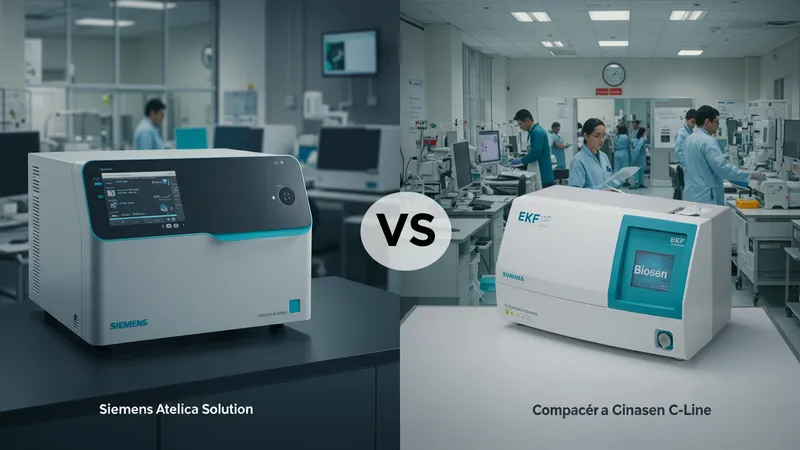
Lower-priced devices like the EKF Biosen C-Line offer an entry point for secondary hospitals or expansion programs looking to extend diabetes care coverage efficiently. Its consumables, such as test strips, are widely available in Mexico and competitively priced, making recurrent costs manageable for facilities serving large populations with limited funding. Reliability and ease of maintenance further reduce operational disruptions, part of why this device is common in both metropolitan and regional clinics.
System integration is another cost-related factor, especially as Mexican hospitals increasingly shift to electronic health records (EHRs). Devices like the Abbott i-STAT Alinity and Cepheid GeneXpert Xpress are designed with advanced connectivity features, enabling seamless transfer of results into patients’ digital charts. This enhances data accuracy, supports telemedicine initiatives, and reduces administrative load—all important for streamlining processes in crowded clinical environments.
When evaluating total cost of ownership, Mexican facilities must consider not only purchase price, but also training, servicing, and the availability of local technical support. Partnerships with vendors who have established service networks and Spanish-language resources can significantly lower timelines for repairs or troubleshooting, ensuring minimal diagnostic downtime in busy wards. The next section delves into specific use cases demonstrating real-world impact across Mexico’s healthcare landscape.
Portable diagnostic tools are reshaping care pathways within Mexican hospitals. In emergency departments, the Abbott i-STAT Alinity expedites blood gas and chemistry testing, enabling clinicians to address critical cases—such as heart attacks or severe sepsis—within minutes of admission. This immediacy can help reduce time-to-treatment metrics, with Mexican hospitals reporting higher patient throughput and fewer lab-related treatment delays as a result.

Hospitals dealing with high caseloads of respiratory diseases have leaned on the Cepheid GeneXpert Xpress’s rapid molecular testing for tuberculosis and COVID-19. Several Mexico City facilities have reported smoother patient flows and enhanced isolation protocols, which are vital for outbreak containment in densely populated areas. By placing these systems at triage points, staff can quickly separate infectious from non-infectious cases, alleviating pressure on inpatient wards.
Multidisciplinary teams benefit from the Siemens Atellica Solution’s capacity to run a broad menu of tests with minimal sample handling, even during peak periods. Physicians in central and northern Mexico have cited improvements in coordinated care for complex cases and reduced dependence on overburdened central labs. As a result, patient turnover improves while maintaining high diagnostic accuracy across multiple specialties.
Portable ultrasound, such as the Dragonfly Mini, finds critical application in regional clinics across Oaxaca and Chiapas, where transport logistics impede timely imaging referrals. By bringing real-time imaging to prenatal, trauma, and cardiac assessments at the point of care, these tools bridge geographical gaps in expertise, empowering frontline clinicians and supporting telemedicine consultations. Next, we’ll investigate the digital integration and future pathways for these innovations in Mexican healthcare.
Digital connectivity is elevating portable diagnostics in Mexico’s high-capacity health system. Devices like the Abbott i-STAT Alinity and Cepheid GeneXpert Xpress are increasingly networked, allowing test results to be transmitted instantly to centralized electronic health records. This not only supports real-time clinical decision-making but also enables remote monitoring by specialists and facilitates efficient public health reporting—essential in a country with widespread urban and rural care points.

Innovation is shaping the next wave of portable diagnostics for Mexican hospitals. Enhanced battery life, wireless connectivity, and improved interfaces are reducing the learning curve for busy medical teams and supporting seamless operation even during mobile outreach campaigns. Collaborations between Mexican universities and manufacturers are also fostering adaptations for local needs, ensuring devices meet both large and small hospital requirements in diverse regions.
The expanding role of telemedicine and digital health platforms in Mexico is closely tied to the integration capabilities of these portable devices. Instant sharing of test results supports consultations across city, state, and rural divides—shortening wait times for specialist input and reducing unnecessary travel for patients. This connectivity is especially significant for multi-site hospital networks and national health programs managing chronic diseases or infectious outbreaks.
As high-capacity healthcare facilities in Mexico continue to implement and scale portable clinical diagnostic devices, the interplay of cost, performance, and digital integration will drive outcomes for millions of patients. These technologies not only enhance efficiency and accuracy in crowded hospitals but also underscore a broader movement toward accessible, equitable healthcare for all, setting the stage for ongoing advancements in Mexican medicine.